COVID-19: Are Mechanical Ventilators Killing People? | The Return of The H-H Inhalator

Could the mechanical ventilators routinely used on COVID-19 patients be killing them? A growing body of evidence says yes. Both the intense pressure and the high levels of oxygen forced into patient’s lungs appear to be responsible for the damage caused by mechanical ventilators, which were first proven harmful in 1827 by French surgeon Leroy d’Etoille. Yet the public health disaster known as mechanical ventilation continues to this day.

In this article I’ll present the evidence suggesting mechanical ventilators are harming patients and doing precisely the opposite of their intended use – reducing cellular oxygenation rather than increasing it. I hope it helps you form your own opinion on the matter.
Carbogen, a mixture of 5% carbon dioxide in either air or oxygen, has been proven to cure pneumonia in 12 to 24 hours and was routinely used by firefighters, hospitals and rescue crews on emergency patients in the United States in the 1940’s.
This is a call to hospitals worldwide for the immediate replacement of mechanical ventilators with HH-Inhalators, devices that produce and administer carbogen gas to patients, which will heal instead of harm. Be sure to pass this article onto any doctors or nurses in your life so they can learn about the virtues of carbogen and why mechanical ventilation is a public health disaster.
TABLE OF CONTENTS
COVID-19 Controversy Surrounding Mechanical Ventilators
In the early days of the COVID-19 pandemic, a dispute broke out among critical care and emergency physicians: could the mechanical ventilators routinely used on COVID-19 patients (and not the virus itself) be the cause of ARDS (Acute Respiratory Distress Syndrome)?
Much of the debate was spurred by the impassioned pleas of the New York-based emergency physician Cameron-Kyle Siddell, who noticed from direct experience treating patients the harm being caused by mechanical ventilation.(1)
“This is the disease—Advanced Respiratory Distress Syndrome (ARDS)—that every hospital is preparing to treat. And this is the disease for which 100,000 Americans might be put on a ventilator. And yet, everything I have seen in the last 9 days [has] led me to believe that COVID-19 is not this disease, and that we are operating under a medical paradigm that is untrue. I don’t know the final answer of this disease, but I’m quite sure that a ventilator is not it.”
– Dr Cameron-Kyle Siddell
“I’ve talked to doctors all around the country and it is becoming increasingly clear that the pressure we’re providing may be hurting their lungs, that it is highly likely that the high pressures we’re using are damaging the lungs of the patients we are putting the breathing tubes in,” continued Siddell.(12)
Reports from Wuhan, Seattle and cities in Italy now suggest that placing patients on ventilators may not significantly improve their chances of recovery or survival at all.
“Contrary to the impression that if extremely ill patients with COVID-19 are treated with ventilators they will live and if they are not, they will die, the reality is far different,” Gillick said.
For decades it has been known that the use of mechanical ventilators themselves can cause pneumonia in patients. One team of scientists wrote that patients undergoing mechanical ventilation “are at significant risk of developing a secondary, ventilator-associated pneumonia (VAP).”(1)
An article from Live Science reported the following:
Patients with low blood-oxygen levels but few signs of distress or organ damage may not benefit from ventilation, according to researchers from Italy and Germany who submitted a letter published March 30 in the American Journal of Respiratory and Critical Care Medicine. In the letter, they described patients with these traits in Italy and Germany, noting that their lungs appeared relatively healthy as compared with COVID-19 patients with acute respiratory distress, a condition where the air sacs in the lungs fill with fluid.
Even if patients do develop acute respiratory distress, they may not benefit from ventilation either. The thick fluid clogging up the lungs “limits oxygen transfer from the lungs to the blood, even when a machine pumps in oxygen,” said Dr. Muriel Gillick, a geriatric and palliative care physician at Harvard Medical School. In this case, placing a patient on a ventilator could damage their lungs by introducing too much pressure into the organ, she said.
Modern doctors are observing what had been proven almost 200 years ago: Mechanical ventilation is a dangerous and damaging practice. In 1827, French surgeon Leroy d’Etoille demonstrated “that elevated air pressure could cause ruptured alveoli, emphysema, and tension pneumothorax.”(13) The elevated air pressure he describes is the same that’s routinely being used today on COVID patients with mechanical ventilators.
If mechanical ventilators are harmful, then why are they being routinely used on COVID-19 patients?
In order to answer this question, it’s essential that we understand a bit about the history of mechanical ventilators. An essay from Harvard University in 2021 details the history of ventilators and how the disease ARDS emerged as a syndrome caused by the use of ventilator technology itself.(2)
Our story begins with the polio outbreak in Copenhagen in the early 1950s.
Ventilators & The Polio Outbreak in Copenhagen
In 1952, Polio struck the city of Copenhagen hard. The emergence of the Polio epidemic in the early 1950’s sparked the revival of a dangerous practice in medicine that had long been proven harmful: Positive-pressure ventilation. The Blegdam, Copenhagen’s only infectious diseases hospital, was quickly overrun with patients, and they needed a way to handle the tsunami of patients “desperately ill with respiratory insufficiency and impairment of deglutition, drowning in their own secretions.”
A closer look at the polio patients reveals that many had respiratory paralysis, where they basically stopped breathing. “Their bold solution was to manually ventilate patients by squeezing a rubber bag attached to a tracheostomy tube inserted through an incision just below the larynx,” reports a study published in The American Physiological Society in 2005.(10) “The logistical problem was solved by having a roster of 200 medical students who operated in relays. At the height of the epidemic, 70 patients had to be manually ventilated around the clock. The medical students worked 6- or 8-h shifts so that three or four shifts were needed in the 24 h.” One report states that 1,500 students in all took part in this activity with a total of 165,000 hours(16).

It’s important to note that no successful treatment by positive pressure ventilation given continuously over a long period had been reported by 1950(12). This is a great example of the dissociation that commonly occurs between scientific advancements and their application to clinical situations. Here we have a procedure that had been proven ineffective and harmful long ago, and yet positive-pressure ventilation was chosen to deal with patients during the Polio outbreak.
By Christmas of 1952, the polio epidemic began to fade, and the mortality rate had dropped from 87% to below 40%. Manual ventilation was hailed “superior to all other methods of artificial respiration in securing adequate ventilation.”(13) To this day, many cite this incident as proof of the effectiveness of mechanical ventilators, but “this is not entirely accurate,” reported Dr. Yvan Prkachin of Harvard University in his 2021 review.(14) According to Lassen, manual ventilation is safer and more effective than mechanical ventilation. Prkachin wrote,
Lassen himself noted in his first report on the 1952 epidemic that one of the greatest advantages of the Copenhagen experiment was the avoidance of mechanical ventilation altogether (in the form of iron lungs) in favor of manual ventilation without machines: “In our experience this new form of positive-pressure ventilation (bag ventilation) can be used continuously for months. … [I]t has in many instances been possible totally to avoid the use of mechanical respirators. This we consider a great advantage.”(13)
Something not mentioned in Prkachin’s paper that’s also critical to understand, as far as the differences between ventilation during polio and ventilation during COVID, is that the air administered to patients in Copenhagen in 1952 contained 50% nitrogen and 50% oxygen, which is significantly less damaging than the 100% oxygen administered under pressure to COVID-19 patients using mechanical ventilators.
The manual ventilation of patients in Copenhagen during the polio outbreak was safer and less harmful than what is being done today on COVID patients, but I maintain that even the manual ventilation of 50% oxygen used on polio patients was doing more harm than good. A major misunderstanding of respiratory physiology in the 50’s, which still exists today, maintains falsely that carbon dioxide is a waste gas. (More about why a high level of carbon dioxide is essential for health shortly.)
Chief physician at the hospital Alexander Lassen (1900–1974) admitted that they didn’t really know what they were doing. “Although we thought we knew something about the management of bulbar and respiratory poliomyelitis it soon became clear that only very little of what we did know at the beginning of the epidemic was really worth knowing”(21).
Mechanical Ventilators: A Public Health Disaster!
One of the common features observed in COVID-19 patients in hospital settings is a rapid oxygen desaturation in the blood. The response by the medical industry has been to administer fentanyl, (which, prior to the COVID-19 outbreak was labelled “The most dangerous illegal drug in America”(55)) then force oxygen into their lungs through the use of a mechanical ventilator. This practice suggests an alarming lack of understanding of human physiology and of history.
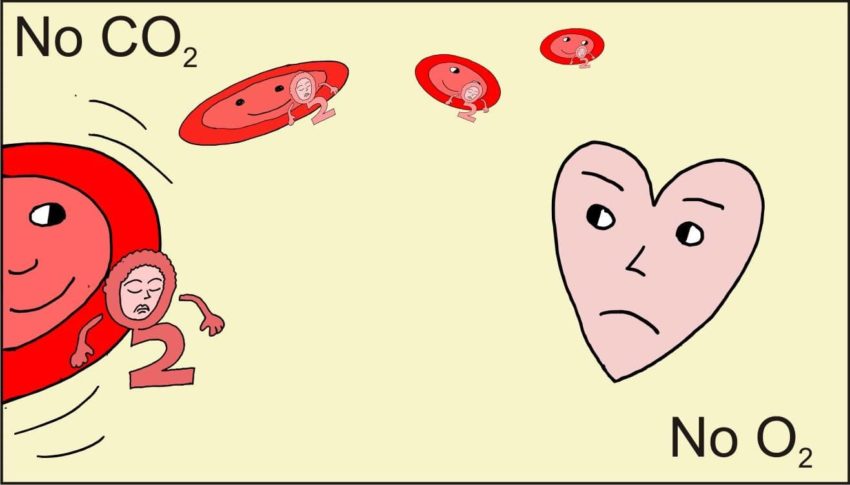
By forcing oxygen into the lungs of patients using a ventilator, carbon dioxide (CO2) gas is rapidly removed from the bloodstream and replaced by oxygen. This would be beneficial if carbon dioxide were actually a waste gas like it’s widely believed to be, however, what’s taught to doctors and nurses in their medical training about the physiological role of carbon dioxide in the body is dead wrong! The fact remains that without adequate carbon dioxide, the body cannot use oxygen, and the keys to understanding why are a couple important concepts called The Haldane Effect and The Bohr Effect.
The Haldane Effect, first described by John Scott Haldane in the early 20th century, shows that elevating blood oxygen levels will remove carbon dioxide from the body. And The Bohr Effect, which is a mirror image of The Haldane Effect, shows us that without sufficient carbon dioxide in the body, the cells cannot use oxygen. By forcing oxygen into the lungs of COVID-19 patients using positive pressure ventilation, oxygen use becomes further impaired, rendering the hypoxia worse.
| “Do people know that our health depends on the level of carbon dioxide in the body?” – Dr Alina Vasiljeva and Dr David Nias |
Is Mechanical Ventilator-Induced Damage Being Blamed on COVID-19?
A mild case of the COVID-19 respiratory illness can include coughing, fever or shortness of breath, no different than the flu. In cases of severe COVID-19 the patient experiences pneumonia.
The symptoms of pneumonia reported in severe COVID-19 patients (ie damaged air sacs in the lungs) are identical to the damage caused by mechanical ventilators. Is this a coincidence? Or is the damage (and deaths) caused by the use of mechanical ventilators being blamed on the SARS-CoV-2 virus? Any doctors working directly with COVID patients who are reading this I’d love to hear your perspective based on your experience.
Whatever the case may be, what’s most important is finding a safe and effective replacement for mechanical ventilators.
It is an honor to introduce to you a miraculous medical intervention that was once commonly used in medicine but has now been forgotten. It’s safe, highly effective for many disorders, and is proven to cure pneumonia in 12 to 24 hours. Carbogen is the perfect remedy to use in place of mechanical ventilators in emergency medicine, especially for COVID-19.
The Return of The HH-Inhalator: Carbogen to the Rescue
Carbogen therapy is the medical administration of a mixture of around 5% carbon dioxide in either air or 95% oxygen to patients in emergency situations. Produced using a device called an H-H Inhalator, carbogen powerfully stimulates breathing and promotes vasodilation in the body. Medical use of carbogen was investigated in the mid-twentieth century for a range of health issues including depression, neuroses, psychoses, dementia, arthritis, cerebral palsy, asthma, hiccups, and whooping cough.
The article Carbon Dioxide by the late Yandell Henderson, discusses the routine use of carbogen by rescue crews in the 1940s generated by a device called an H-H Inhalator. Treat a patient with pneumonia using an H-H Inhalator and a rapid recovery will be induced.
“A special form of apparatus, the H-H Inhalator, for the administration of a mixture of oxygen and carbon dioxide to asphyxiated patients was, therefore, devised and has been widely introduced. This treatment has been so successful that many thousands of these inhalators are now in use: several hundred, for instance, in metropolitan New York, and a number corresponding to the population in Chicago and other cities. The rescue crews of the fire and police departments, the gas and electric companies, and now also the hospital ambulances generally have them. At first a mixture of 5% carbon dioxide in oxygen was used, but 7% has proved even more beneficial. The value of this treatment is not merely for the saving of life, but also for the prevention of such postasphyxial sequelae as pneumonia, injury to the heart, and permanent nervous impairment. In many cases of brief but intense asphyxiation the patient is completely restored within an hour; he may then voluntarily and safely go back to work.”
– Dr Yandell Henderson
Rather than administering pure oxygen to patients using mechanical ventilators and reducing cellular oxygenation by purging the valuable CO2 from their bodies, Carbogen rapidly oxygenates cells, which is exactly what patients lacking oxygen need.
Pneumonia Cured in 24 Hours Using Carbogen
One of the hallmarks of severe COVID-19 infection is pneumonia and the difficulty breathing (dyspnea) and inflammation-induced damage of the alveoli in the lungs. Severe COVID-19 is pneumonia, and a cure for pneumonia has been known for almost 100 years.
In the 1930s, Dr. Yandell Henderson reported to completely cure dogs with pneumonia in just 12 to 24 hours through the administration of carbogen.(20). It worked on dogs and on humans.
“Many cases of pneumonia have now been treated with inhalation of carbon dioxide in oxygen; and a special tent for this treatment is being introduced by Henderson and Haggard. It is believed by those who have used it that this treatment is decidedly superior to that with oxygen alone,” wrote Dr. Henderson.
One last thing I’ll cover before wrapping up this work is the question: If carbogen is so effective, why did the world stop using it? I reached out to Dr. Ray Peat for an answer, to which he wrote:
“The reason that carbogen has hardly been used during the last 65 years is that a British government committee declared, without any evidence at all, that its use was irrational and harmful. The patients’ problem was not getting enough oxygen, and even if their blood pH measurements were right, which is questionable, a low pH from high CO2 is protective against oxygen deprivation. Peter Stewart’s contribution to respiratory physiology still hasn’t been assimilation by the medical profession.”
– Dr. Raymond Peat
Conclusion
Historic and scientific evidence show us clearly that the administration of oxygen under pressure causes damage to patients. Let us take this as a reminder that when we refuse to learn from history, we do so at our own peril. The current public health disaster of mechanical ventilating COVID-19 patients has been wrought by our own ignorance and the havoc is playing out now in emergency rooms worldwide.
A tried, tested and true medical intervention that should replace the use of positive pressure ventilation of pure oxygen is carbogen. The 5% carbon dioxide gas in 95% oxygen mixed by the HH-Inhalator was proven almost 100 years ago to rapidly cure pneumonia – the exact condition seen in severe COVID-19 patients. The evidence suggests a return to carbogen administration on COVID-19 patients and also in place of pure oxygen in all emergency situations.
This article is a call for the immediate replacement of the practice of mechanical ventilation with carbogen mixed and administered by the use of the HH-Inhalator.
Thank you for reading. For more articles, be sure to subscribe to our newsletter at www.endalldisease.com/subscribe
